What Are Memory Care Services?
“Memory care services are a type of support designed specifically for people living with Alzheimer’s and other forms of dementia. This can be in a nursing home, assisted living or care at home.”
Here’s something that might surprise you: Almost 90% of older adults want to stay in their homes as they age.
That’s according to AARP.
But here’s the tough truth—many of them won’t just need help with cooking or getting dressed.
Some will face something much harder: dementia. And that’s where memory care services come in.
What We’ll Cover:
So, What Is Memory Care?
Memory care services are a type of support designed specifically for people living with Alzheimer’s and other forms of dementia. This can be in a nursing home, assisted living or at home.
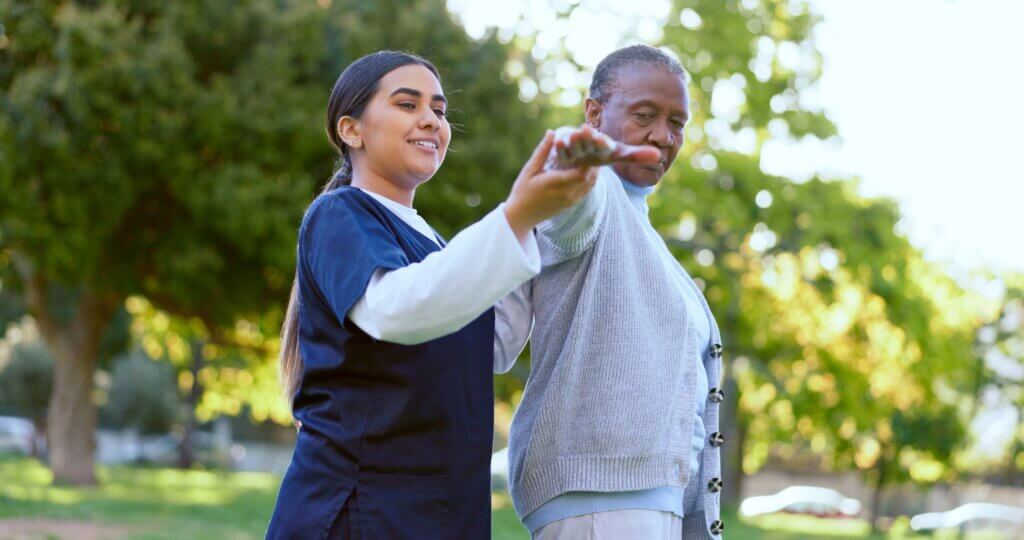
It’s not just about having someone around to help—it’s about creating a safe, structured, and understanding environment where someone with memory loss can live with dignity and as much independence as possible.
Think of it this way: traditional home care might help your mom take her medication or get dressed. They are great at what we call ‘dementia lite’ care.
True memory care? It’s about understanding why she suddenly thinks her childhood friend is coming over for lunch—or why she’s trying to leave the house at 10 p.m.
It takes a different kind of patience. A different kind of training. A different kind of care.
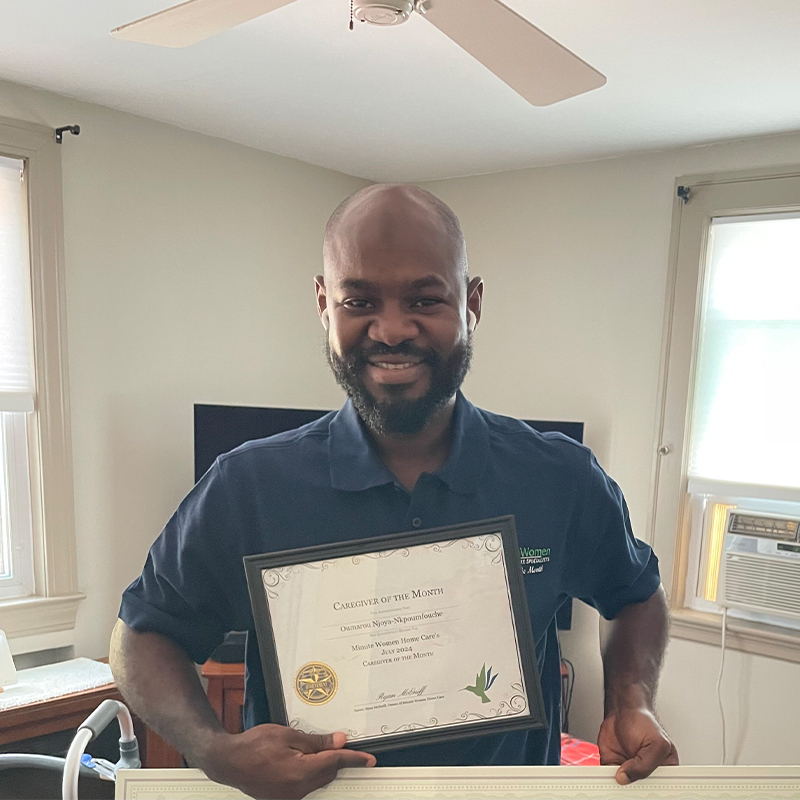
At Minute Women Home Care, we call our team Memory Care Professionals—and that’s not just a title.
It means every caregiver is trained specifically in how to care for someone with dementia. And that training? It matters because you can’t redirect hallucinations or manage sundowning if you haven’t been taught how.
How Memory Care Works (And Why It’s Different)
We start with one important principle: live in their reality.
That means we don’t argue. We don’t correct. We don’t remind someone, “that person passed away years ago.”
We meet them where they are—emotionally, mentally, and physically. It’s called person-centered care, and it changes everything.
Let me tell you a story.
One of our clients, Lisa, was sharp, strong-willed, and didn’t think she needed any help.
Her daughter was exhausted, trying to keep her safe while working full time. When we stepped in, we didn’t start with a completed care plan. Her daughter was too exhausted and overwhelmed to provide all the necessary information we would like to have before starting services.
So what did we do?
We started with listening. What did Lisa love? What made her laugh? What music did she play while cooking for her kids? What did she cook for her kids most often?
That personal history helped us build a care routine that worked for her, not for a textbook. And within a few weeks, we weren’t just memory care professionals — we were trusted companions.
We can help you find expert-level dementia care for your aging parents
Where Can You Find Memory Care Services?
You’ve got two main options:
1) In a facility (like assisted living or nursing homes):
- These often have “memory care neighborhoods”—separate wings with added security, staff, and structure.
- In Boston, expect to pay $8,000 to $14,000 per month, depending on the bells and whistles.
- Medicaid may help only if it’s a nursing home. But many families prefer to avoid that route.
2) At home (like what we do at Minute Women):
- Personalized, one-on-one support right in the comfort of your home.
- More flexible. More familiar. Often better for those who get confused in new environments.
- The cost? Around $45-55/hour, depending on the complexities of the case. Less if it’s non-specialized care, but this level of expertise matters.
Let’s do the math: if you need fewer than 60 hours of care per week, in-home memory care is usually cheaper than a facility.
More than that? It gets expensive.
But here’s the kicker—many assisted living places still require private care on top of their services once your loved one declines.
In fact, about 35% of our business is supporting families who have already moved into assisted living.
Who Pays for Memory Care?
Coverage is where it gets tricky. Medicare doesn’t cover it. Not at home. Not in assisted living. Not in memory care units.
If you qualify for Medicaid, it might help in a nursing home—but that’s often not what families want.
The only insurance that really helps is long-term care insurance, and even then, it depends on your policy. If you’ve got it—great! If not? Expect to pay out of pocket.
Contact us today for a fast, friendly conversation about your loved one’s needs
Why Memory Care Services Are Worth It
Dementia is hard. It’s hard on families. It’s hard on relationships. But memory care—real memory care—can make it easier.
It means your dad isn’t scared or confused by strangers. It means your mom gets to hear her favorite Elvis song while folding towels and smiling. It means fewer falls, fewer meltdowns, and more moments of connection.
Most importantly, it means you get to be a daughter again. Or a son. Not just the family caregiver.
Here’s the real difference between regular home care and memory care—it’s not just about helping someone get dressed or prepping a meal. It’s about deep understanding, consistency, and transforming how families experience life with dementia.
Let’s break it down:
1) Caregivers Who Understand Dementia
You’re not just hiring help. You’re bringing in a team that knows the disease.
Our memory care professionals are trained specifically in dementia care—they know how to respond when your mom asks the same question five times in ten minutes.
They’re not rattled by wandering, paranoia, or mood swings. In fact, they’re prepared for it. That changes everything.
2) Consistency You Can Count On
Dementia thrives on routine. So does good care.
We prioritize the same caregiver on the same days, at the same times—because that consistency creates comfort. Familiar faces. Familiar voices.
It lowers stress and makes your loved one feel safe. And for you? It means no guessing, no last-minute changes, no chaos.
3) More Than Care—A New Quality of Life
This benefit is where memory care shines.
With the right support, your loved one can still laugh, connect, and enjoy the small moments.
It’s a total solution that enables a quality of life with dementia that families didn’t know was possible.
We’ve had families look at us after a few weeks and say, “We thought we had lost her—but she’s smiling again.” Memory care services don’t just manage symptoms. It opens the door to joy, safety, and connection—even in the hardest moments.
Key Takeaways
Memory care services aren’t just another layer of senior support. They’re a lifeline for families trying to keep their loved ones safe, connected, and at home.
If your parents are showing signs of dementia—forgetfulness, confusion, agitation—don’t wait until there’s a crisis.
Ask questions. Get support. Build a plan.
And if you’re not sure where to start? Call us. We’re happy to just talk. No pressure. No sales pitch. Just a conversation that might make your life a little easier—and your loved one’s a lot safer.
Call us to learn how our in-home dementia care specialists can help!
About Us
Minute Women is a premium, non-medical, in-home dementia care service provider. We assist our clients with activities of daily living so they can live at home with dignity and respect. We also support families in their mission to age in place rather than transition to a nursing facility.
Connect With Us